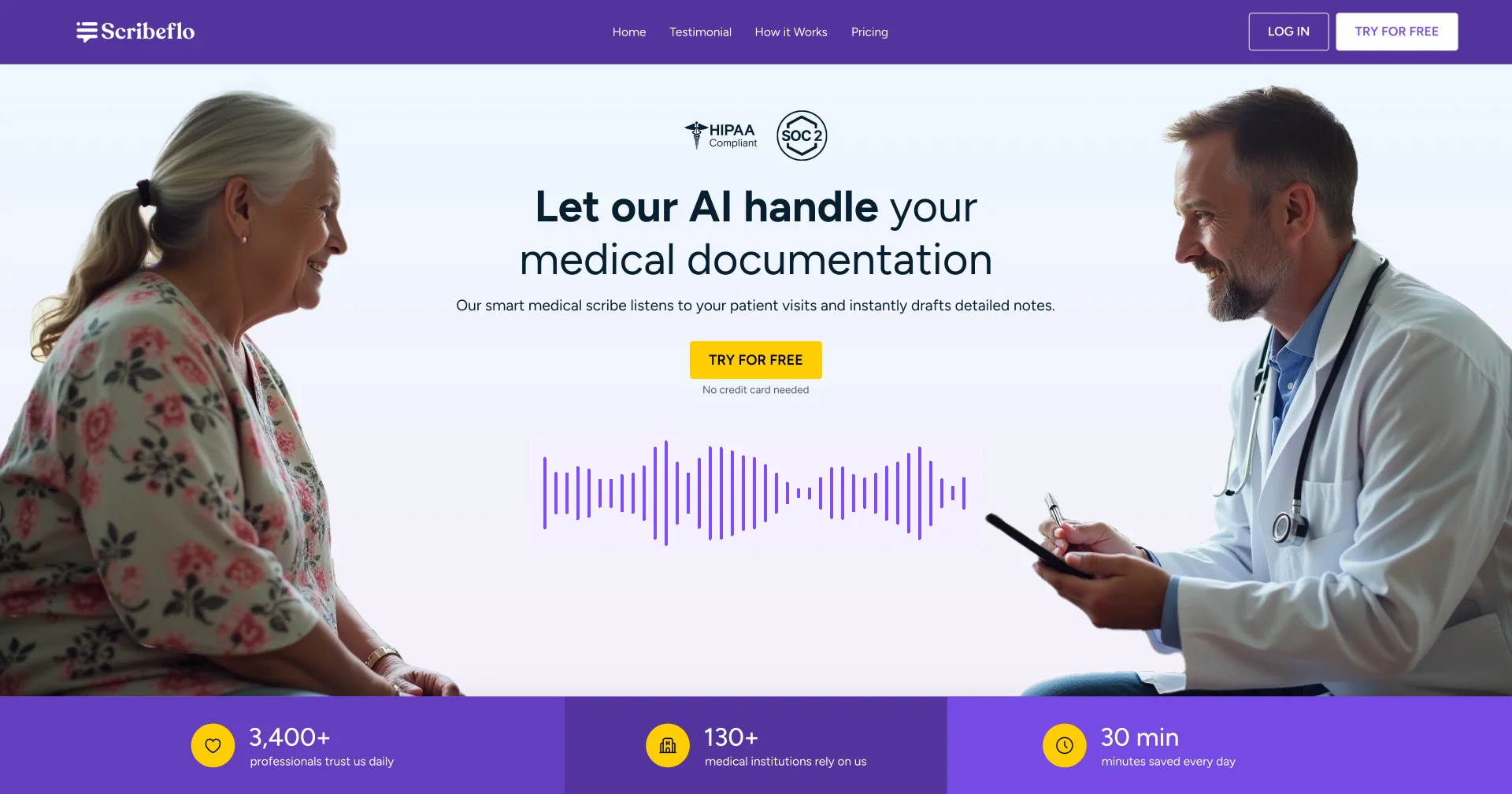
About the project
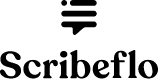
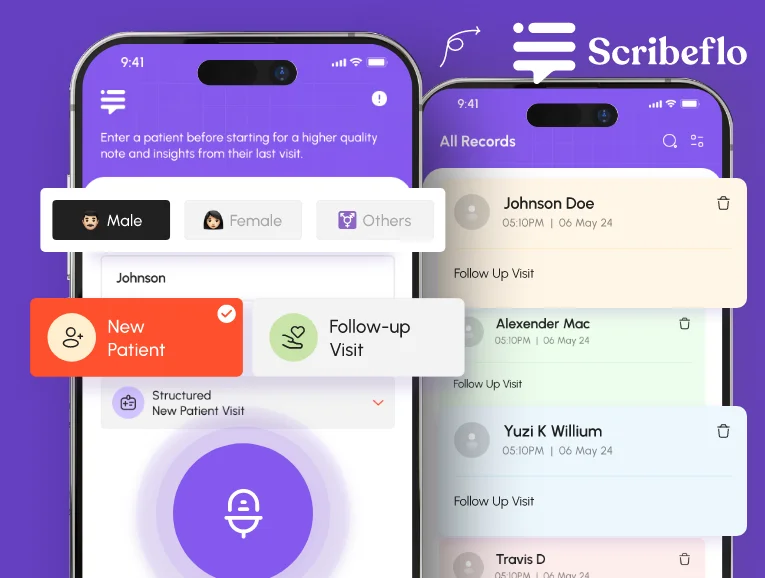
Scribeflo is an AI-powered medical scribe platform built to help physicians, therapists, and clinicians automate clinical documentation. It listens to patient consultations in real time, transcribes conversations with medical accuracy, and generates structured SOAP notes, enabling faster workflows, improved compliance, and reduced administrative burden.
Challenge
The healthcare industry faces mounting documentation burdens, with clinicians spending excessive hours on manual note-taking instead of patient care. Existing transcription tools lacked real-time accuracy, contextual understanding, and compliance readiness. Recognizing this inefficiency, Codiant identified an opportunity to build Scribeflo - an AI-powered scribe transforming clinical documentation through automation and intelligent workflow optimization.
Approach
Codiant’s product, design, and AI engineering teams collaborated through an agile development framework to transform the concept into a deployable healthcare solution. The process began with in-depth research on clinical workflows, followed by feature prioritization around transcription accuracy, data privacy, and usability. Continuous iteration, real-world testing, and clinician feedback shaped Scribeflo into a market-ready product.
Discovery phase
In 2024, we began exploring how AI could simplify healthcare documentation. Through research and clinician interviews, we identified three key problems—excessive administrative workload, lack of real-time transcription tools, and inconsistent data accuracy. These findings guided us to design Scribeflo, an AI scribe that automates note-taking, ensures compliance, and saves valuable clinical time.
Market Research
$8.76 billion by 2032
is the projected global market size for AI-based medical transcription software, growing at a 16.7% CAGR.
60% of clinicians
reported spending over three additional hours daily on manual documentation, increasing burnout and reducing patient care time.
$4.2 billion+ savings
could be achieved annually across US healthcare systems through AI-enabled documentation and workflow automation.
The Gap
Clinicians faced fragmented tools that captured speech but didn’t integrate documentation workflows or comply with clinical context. Existing solutions lacked a unified, AI-driven engine for real-time transcription, structured output and workflow automation. Scribeflo fills that space by combining ambient voice capture, intelligent structuring and clinical workflow integration.
Audience Struggles
Documentation Overload: 44.9% of physicians’ work time was spent on EHR input, not direct patient care.
After-hours Burden: 76.1% of office-based physicians reported spending more than 1 hour per day on documentation outside clinic hours.
Resource Drag: Clinicians were spending 13.5 hours per week generating clinical documentation - over a third of average working hours.
Opportunity
Clinical professionals faced growing inefficiencies from manual note-taking and fragmented transcription tools that lacked real-time accuracy, automation, and affordability. Scribeflo bridges this gap through a unified AI platform that streamlines documentation, reduces administrative burden, and scales effortlessly across healthcare practices delivering measurable efficiency, cost savings, and workflow automation.
Execution Timeline
1. Research & Discovery
2. Structure & Concept
3 Weeks3. Design & Prototyping
4 Weeks4. Development & Testing
6 WeeksResearch Phase
Codiant’s discovery process involved deep market, business, and user research to validate the growing pain of documentation overload. Insights from physicians and clinical administrators revealed adoption barriers centered on usability, compliance, and integration costs. These findings shaped Scribeflo’s focus on simplicity, accuracy, and secure automation tailored to real-world clinical workflows.
Clinical Workflow Insights
Healthcare professionals manage multiple administrative and clinical responsibilities daily. The table below highlights their most common workflow challenges and how Scribeflo transforms them into practical opportunities for efficiency, accuracy, and improved patient care.
| Tasks | Emotions | Challenges | Opportunities |
|---|---|---|---|
| Patient Consultation | 😫 Overwhelmed | Manual note-taking splits attention between patient and screen. | AI transcription captures every detail automatically, keeping full focus on patient care. |
| Note Structuring | 😩 Fatigue | Converting free-form notes into SOAP format is repetitive and slow. | Automated SOAP notes organize conversations into structured summaries instantly. |
| EHR Documentation | 😤 Stress | Manual data entry leads to errors and documentation delays. | One-click EHR export removes redundancy and ensures consistency. |
| Review & Editing | 😕 Pressure | Reviewing each line for accuracy consumes valuable time. | Smart draft editor suggests refinements and accelerates approval. |
| Follow-Up Preparation | 😔 Exhaustion | Difficult to recall key visit details for summaries. | Auto-generated summaries highlight next steps for seamless follow-ups. |
| Compliance Management | 😟 Concern | Manual workflows increase compliance and privacy risks. | HIPAA-compliant system ensures secure documentation automatically. |
| Team Collaboration | 😓 Coordination Stress | Sharing updates across teams lacks central visibility. | Cloud-based sharing gives real-time, role-based access. |
| Reporting & Analysis | 😫 Burnout | Preparing reports manually takes hours of admin time. | Automated report generation simplifies audits and performance tracking. |
User Persona Development

Dr. Adrian Walker
38
Internal Medicine Physician
Boston, USA
Persona Snapshot:
A time-pressed clinician seeking to reduce after-hours documentation and reclaim patient-facing time through automation and workflow efficiency.
Goals:
Reduce time spent on documentation by at least 50%.
Improve daily patient throughput without compromising care quality.
Maintain compliance and accuracy in all clinical notes.
Challenges:
Manual charting consumes significant after-hours time.
Existing transcription tools lack contextual accuracy.
Documentation delays impact billing and patient follow-up.
How Scribeflo Helps:
- Real-time transcription automates note creation, cuts documentation time, and reduces burnout.
- AI-generated SOAP notes ensure accuracy, improve compliance, and enhance clinical reliability.
- HIPAA-secure cloud storage simplifies access and safeguards patient information.

Sarah Nguyen
45
Clinical Operations Manager
Seattle, USA
Persona Snapshot:
An operations leader focused on optimizing clinic efficiency, reducing administrative workload, and improving provider satisfaction through AI-driven automation.
Goals:
Streamline documentation workflows across departments.
Enhance operational efficiency and reduce staff burnout.
Ensure all records meet compliance and audit standards.
Challenges:
Disconnected documentation systems slow down reporting.
High transcription costs impact operational budgets.
Limited visibility into clinician productivity metrics.
How Scribeflo Helps:
- Automated transcription and note generation reduces manual workload and turnaround time.
- Centralized, structured documentation improves operational oversight and audit readiness.
- Real-time workflow analytics enable data-backed resource allocation decisions.
Ideation
Persona research revealed clinicians’ biggest struggle—documentation fatigue and lost time between appointments. Our brainstorming focused on how AI could listen, understand, and summarize naturally without disrupting patient flow. The UX direction prioritized speed, medical accuracy, and minimal interaction. Early prototypes explored ambient listening and adaptive note structures, aiming to reduce clicks, simplify editing, and ensure every note felt effortless yet precise.
User Flow
Wireframing
Feature Concepts
1. Real-Time Transcription
Instant, Accurate, Effortless: Scribeflo captures patient–clinician conversations in real time with high medical accuracy, allowing doctors to focus on care instead of typing notes.
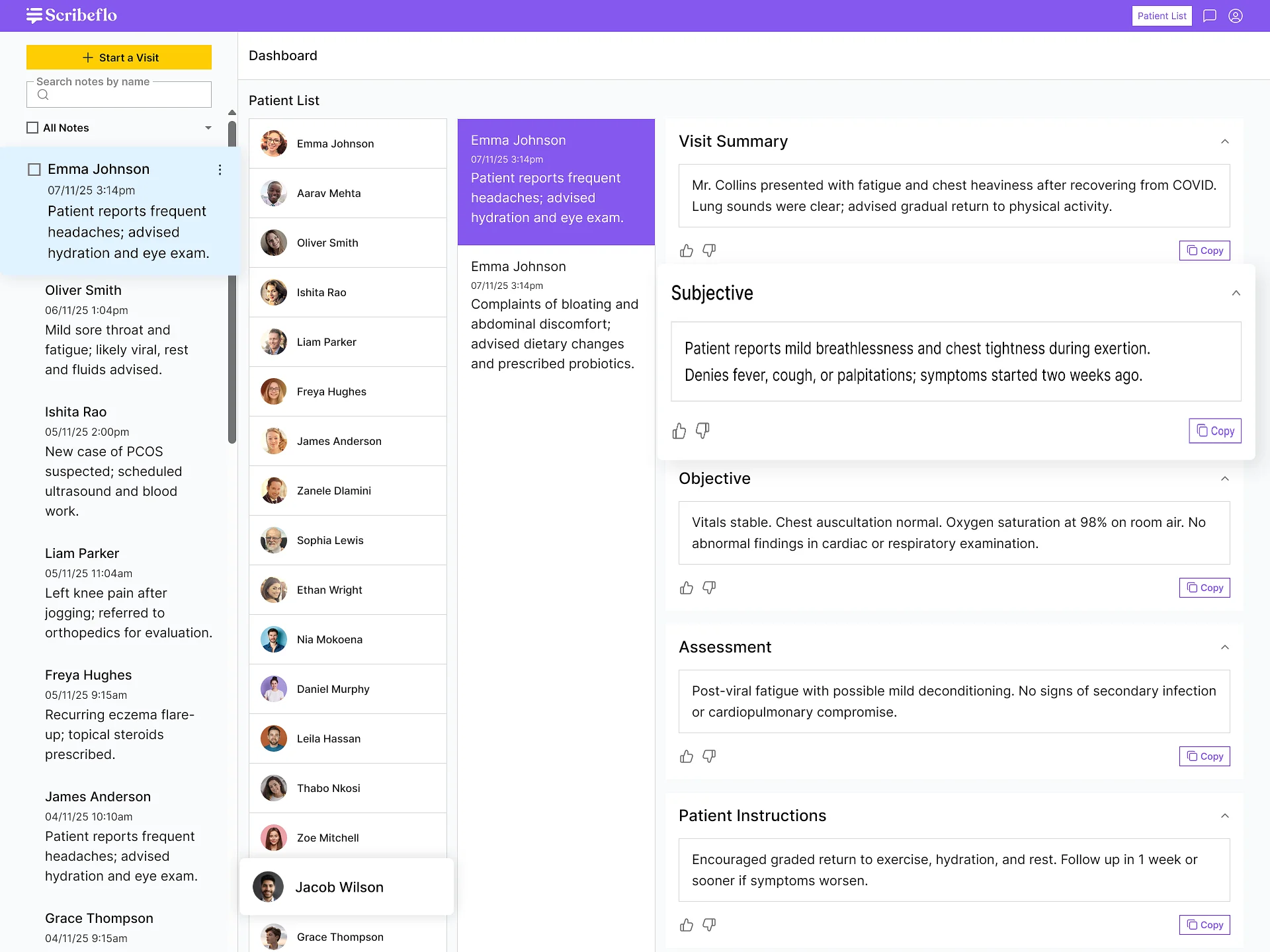
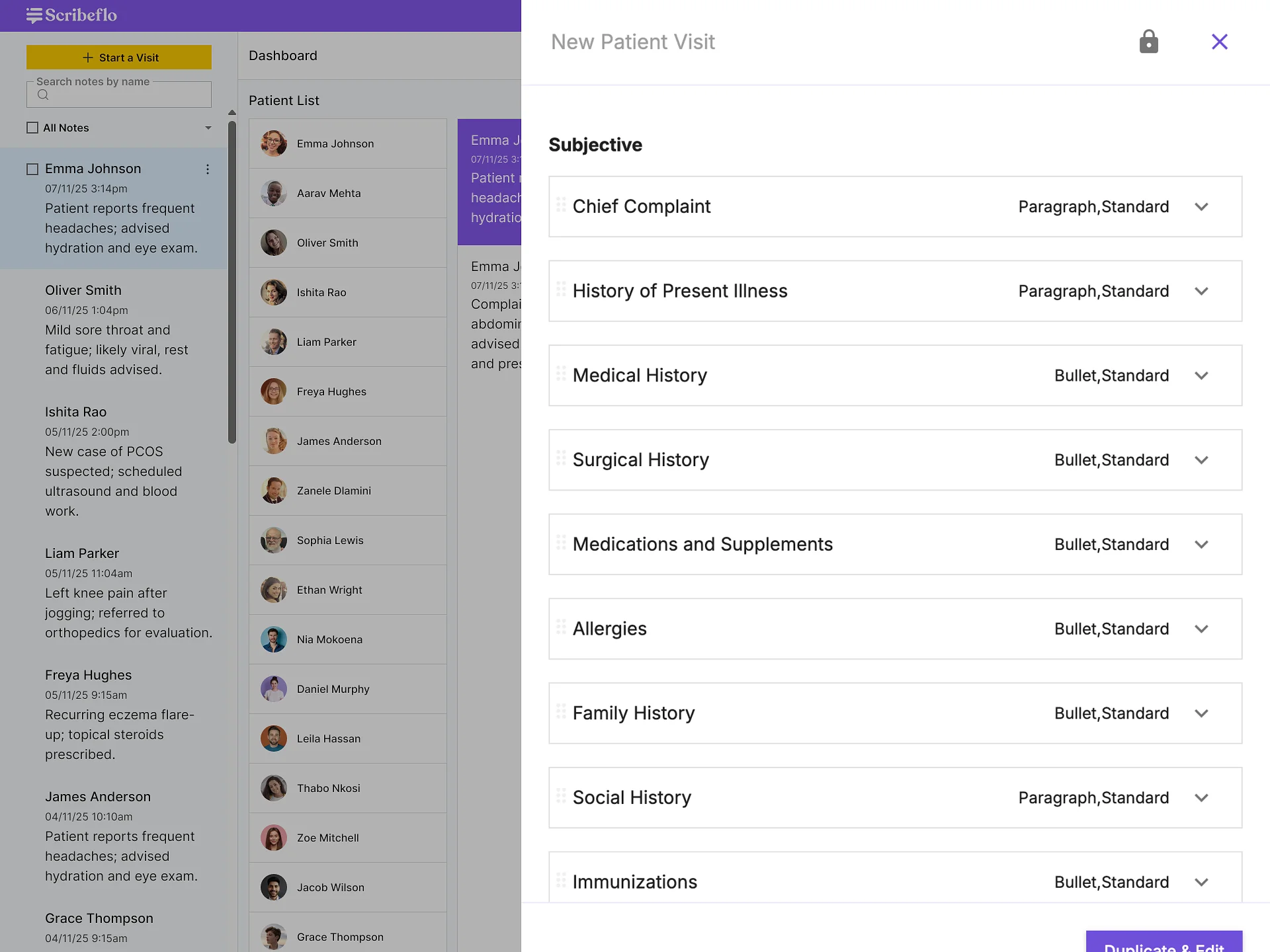
2. AI-Generated SOAP Notes
Structured Documentation in Seconds: Automatically generates Subjective, Objective, Assessment, and Plan summaries after each consultation—ready for quick review and export.
3. Ambient Voice Capture
Hands-Free Recording: Records conversations passively during patient visits, ensuring natural dialogue flow without disrupting clinical interactions.
4. Editable Draft Notes
Review and Refine Instantly: Clinicians can edit, verify, or annotate AI-generated drafts before final submission or upload to EHR systems.
5. HIPAA-Compliant Data Security
Secure by Design: All voice data and notes are encrypted end-to-end, ensuring compliance with healthcare privacy standards.
6. Multi-Device Access
Work Anywhere: Access Scribeflo across mobile, tablet, or web, keeping notes synced and available securely in real time.
7. Workflow Time Savings
Efficiency That Scales: Reduces manual documentation time by up to 60%, enabling faster patient turnaround and lower administrative costs.
8. Structured Note Export
Ready for EHRs: Export finalized SOAP notes or reports in standardized formats for seamless integration into existing healthcare systems.
9. Intuitive User Interface
Built for Clinicians: Clean, distraction-free design reduces cognitive load, supporting faster adoption and improved user satisfaction.
10. Secure Cloud Storage
Always Accessible, Always Protected: Automatically stores all notes in an encrypted cloud, ensuring data integrity and easy retrieval when needed.
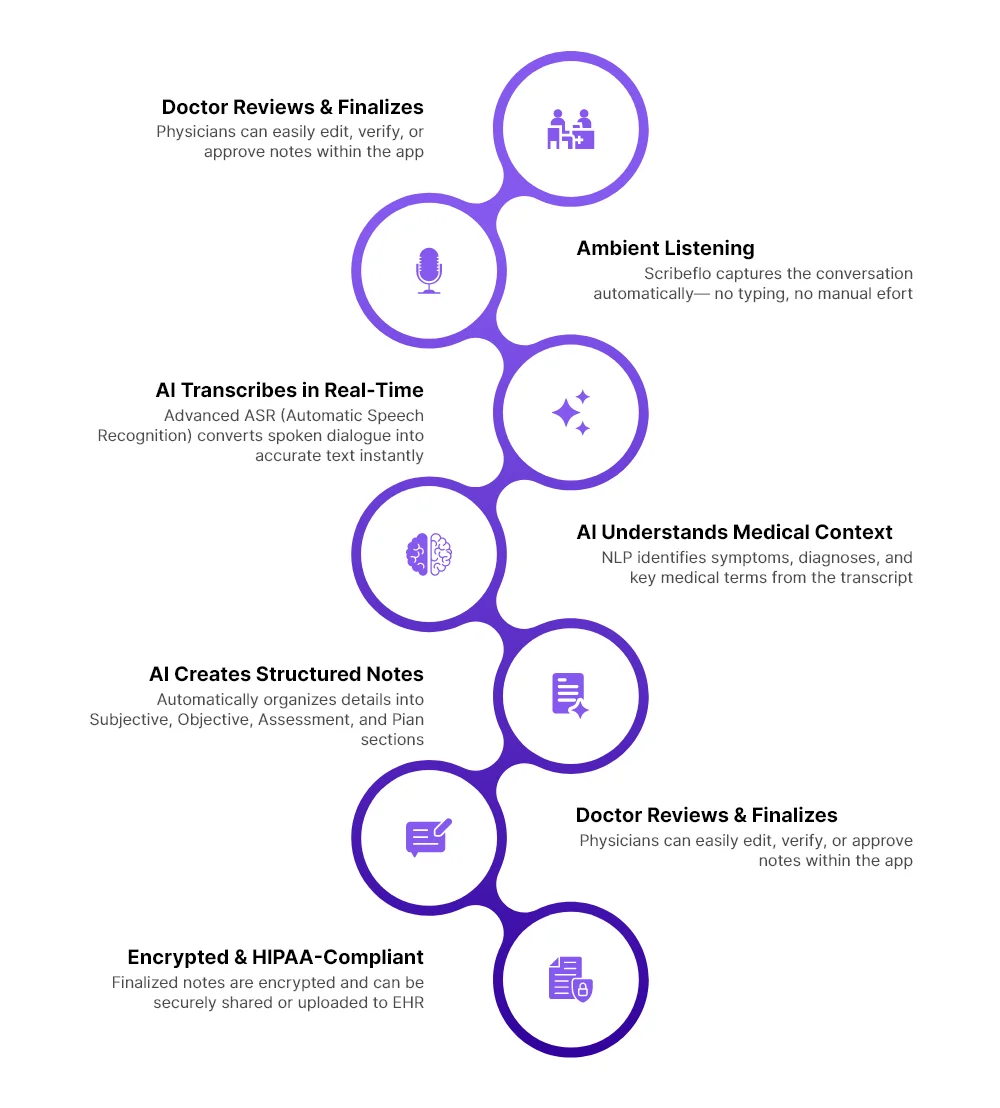
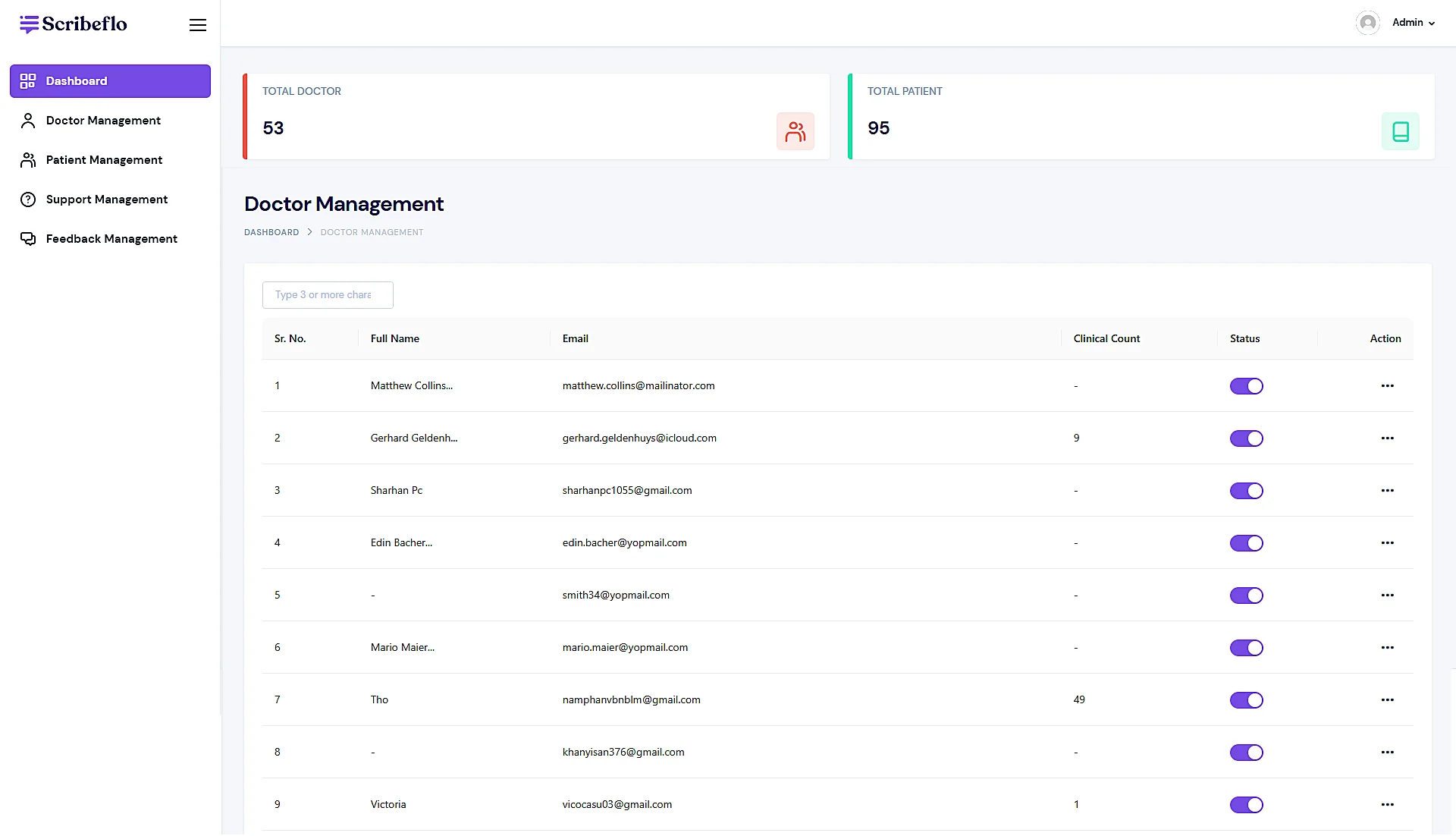
High fidelity designs
Development
To ensure Scribeflo met the demanding standards of modern healthcare environments, Codiant’s engineering team selected a scalable, secure, and high-performance tech stack. The focus was on enabling real-time audio processing, intelligent documentation, and seamless user experience while maintaining full compliance with healthcare regulations.
 React JS
React JS Flutter
Flutter PostgreSQL
PostgreSQL MySQL
MySQL Figma
Figma Illustrator
Illustrator Photoshop
Photoshop Node.js
Node.js Python
Python AWS
AWS OpenAI
OpenAI Transcribe Modal OpenAI
Transcribe Modal OpenAI FastAPI
FastAPIAI-Powered Transcription Core: Built using OpenAI’s Transcribe model for high-accuracy speech recognition and GPT-based contextual understanding, enabling real-time, medical-grade transcription of patient consultations.
Backend Architecture: Built with Python with FastAPI, providing scalable API services, seamless data handling, and fast integration with healthcare management systems.
Frontend Framework: Engineered using React JS and Flutter to deliver a responsive, device-agnostic experience across web and mobile interfaces with consistent performance.
Data Storage & Management: Supported by PostgreSQL databases for reliable, structured data organization, ensuring integrity, scalability, and compliance with healthcare standards.
Design & Prototyping Tools: Crafted using Figma, Illustrator, and Photoshop to design intuitive clinician interfaces that minimize cognitive load and enhance workflow fluidity.
Cloud Infrastructure: Deployed on AWS, ensuring encrypted cloud storage, robust data protection, and seamless scalability across healthcare networks and multi-clinic deployments.
The result
Codiant successfully delivered Scribeflo as a fully functional, HIPAA-compliant AI medical scribe platform built to automate and streamline clinical documentation. The solution combined real-time transcription, structured SOAP note generation, and intuitive editing—empowering clinicians to shift focus from paperwork to patient care.
Within weeks of internal rollout, early adopters reported a 60% reduction in documentation time and a 35% improvement in overall workflow efficiency. The intuitive interface and ambient voice capture minimized after-hours charting, while secure cloud architecture ensured data integrity and compliance across multi-specialty practices.
From a business standpoint, Scribeflo achieved scalability through modular architecture and multi-device accessibility, enabling seamless deployment across clinics of varying sizes. The platform also enhanced provider satisfaction scores by 40%, demonstrating measurable ROI through operational efficiency, accuracy, and reduced burnout.
Scribeflo now stands as a benchmark solution in AI-driven healthcare automation—translating complex clinical interactions into structured, reliable, and ready-to-review documentation in real time.