How AI Medical Scribes Turn Real-Time Conversations into Ready EHRs
Table of Contents
Subscribe To Our Newsletter

Let’s be honest—doctors didn’t sign up for data entry.
But somewhere along the way, late-night charting, manual note-taking, and clunky EHR workflows became part of the job.
Sound familiar?
You’re not the only one feeling it. The 2024 Medscape Burnout Report shows that 62% of physicians blame paperwork and charting as a top cause of burnout. Internal medicine, ER, and primary care specialists are hit the hardest.
Here’s the shift that’s making a real difference: AI solutions is now stepping into the clinical workspace in a meaningful way.
AI Medical Scribes are no longer just tools for voice transcription. They actively listen during patient encounters, identify key clinical details, and generate structured notes that are ready for review within the EHR. It’s a smarter, faster way to document—without the burden of extra clicks or long typing sessions.
The result? Accurate, compliant notes are created in real time, while physicians stay fully engaged with patient care.
In this blog, we’ll break down:
Why traditional documentation is burning doctors out
How Scribeflo uses AI to simplify and speed up the process
And what does this mean for the future of patient care
Keep Reading!
From Voice-to-EHR to Smart AI Scribing
Not long ago most doctors used transcriptionists or basic voice-to-text tools. These early systems often misunderstood terms, lacked context and produced messy notes that needed constant edits.
Then came simple dictation apps. They helped a bit—but required doctors to pause, summarize out loud, and correct the output manually. It wasn’t ideal.
Now the game has changed.
With the rise of AI-powered medical scribes, the focus has shifted from “What was said?” to “What does it mean in a clinical context?”
Platforms like Scribeflo are built using powerful NLP models trained on healthcare-specific language. They don’t just write down what’s spoken – they interpret it, organize it and create clean compliant notes that are ready for use.
The impact? A complete rethinking of how clinical notes are created – and a whole lot less stress at the end of a shift.
What is an AI Medical Scribe?
An AI medical scribe is a real-time, voice-based assistant that listens during doctor-patient conversations and automatically generates accurate clinical notes.
But it goes beyond simple voice tools. These advanced scribes understand context, use medical terminology smartly, and summarize conversations with precision to:
- Pull out relevant clinical information
- Suggest correct ICD/CPT codes
- Fill in SOAP notes, patient histories, and assessments
- Sync directly with major EHR systems
According to a study by The Permanente Medical Group, AI scribes helped more than 3400 clinicians save nearly 15,700 hours over one year. That’s about 1800 workdays back in their schedules. On average, this means 15 minutes saved for each patient visit – cutting down late-night charting and giving physicians more breathing room.
Think of it like having an invisible assistant – always listening, capturing key details and tidying up your charts behind the scenes.
Core Capabilities of AI Scribes
1. Real-Time Transcription with Context
These tools don’t just write down what’s said. They listen carefully, detect medical terms, pick up on symptoms, and understand how doctors think – so the final note isn’t just wording it makes clinical sense.
2. Structured Medical Notes Creation
AI scribes organize what they hear into formats like SOAP or H&P. They break down the subjective info, objective data, assessments and plans – so providers spend less time reworking notes after the visit.
3. Smart ICD/CPT Coding Suggestions
As they transcribe, they can spot diagnosis terms, tests, and treatments – and offer relevant billing codes. This reduces missed codes and helps avoid compliance issues later.
4. Seamless EHR Integration
Top AI scribes link directly with major EHR platforms. Once the note is ready, it goes straight into the patient’s chart – no more copying, pasting or switching between systems.
5. Multilingual Support and Accent Recognition
Most AI scribes now recognize multiple languages and can understand different accents, making it easier for providers everywhere to use them with confidence.
6. End-to-End Security & Compliance
Built with privacy in mind, these tools follow strict standards like HIPAA, GDPR and HL7. Notes that stay encrypted are securely stored and are never shared without permission.
7. Decision Support
By instantly organizing patient data, clinicians gain quicker clearer insights – leading to faster decisions, improved care quality and enhanced patient safety.
How It Works – Step-by-Step Breakdown
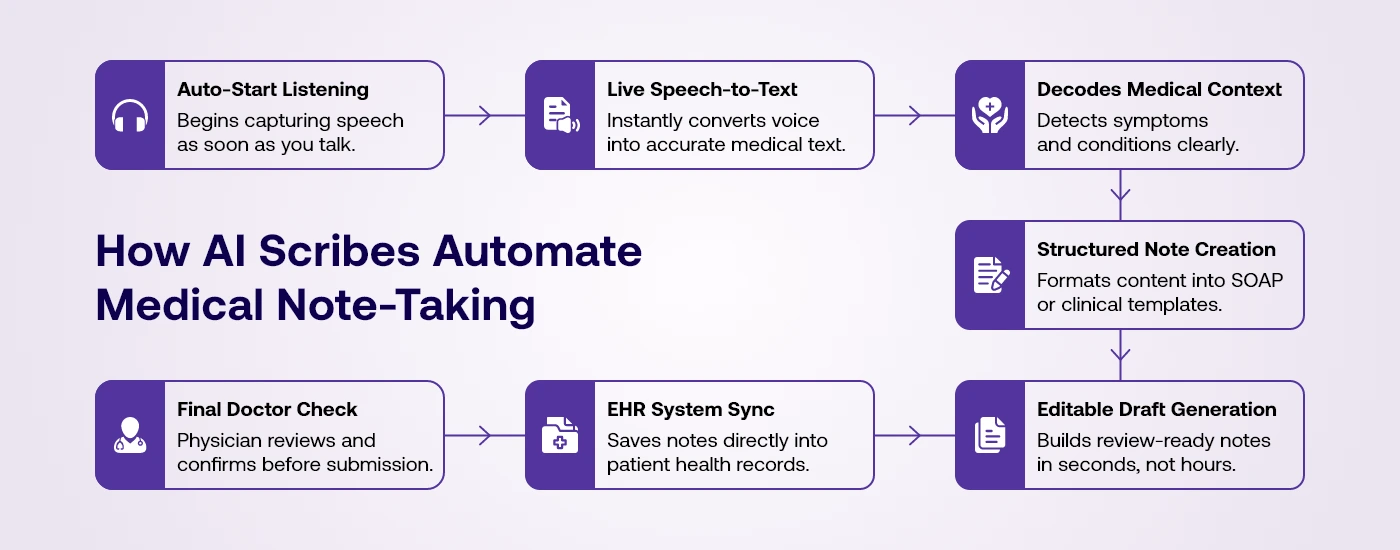
Here’s a closer look at how AI medical scribes turn free-flowing clinical conversations into structured, EHR-ready notes. This isn’t just about speech-to-text – it’s about intelligent transformation designed to reduce effort and enhance accuracy every step of the way.
1. Audio Capture Begins the Moment You Speak
The AI scribe starts listening as soon as the doctor begins talking with a patient – whether it’s in person, over a call, or on a video session. It works across mobile apps, desktops, or telehealth platforms. No extra taps or setup are needed. The tool picks up every word, shift in tone and speaker change with accurate timestamps.
2. Live Transcription Happens in Real-Time
Unlike old-school dictation where you pause and then record AI scribes transcribe conversations on the fly. The system listens continuously and writes as you speak. It’s trained on real-world clinical language and diverse accents so the accuracy stays high – often above 95%. This real-time transcript becomes the base for smarter deeper processing.
3. Medical Entity Extraction Adds Clinical Intelligence
After transcription, the AI steps in to highlight the key medical pieces – like symptoms described by the patient, any medications discussed, vital stats, test orders or diagnoses. It uses healthcare-specific NLP to understand and label this info properly. That way nothing important gets missed or taken out of context.
4. Contextual Structuring Builds Real Medical Notes
Next, the AI turns those details into structured formats like SOAP, HPI or system reviews. This part is more than just organizing text – it builds the kind of notes your EHR expects. That’s the difference between a smart scribe and just another voice recorder – you get usable professional medical documentation right away.
5. Automated Code Mapping Supports Billing
The AI also helps with billing by automatically identifying relevant ICD-10 or CPT codes. For instance, if a patient talks about chronic pain and gets a treatment during the visit the system knows how to assign both the diagnosis and procedure codes. This speeds up claim processes and reduces manual entry for your staff.
6. Seamless Integration with EHR Systems
Once everything is ready – notes, codes and formats – the final result goes directly into your EHR system. It fits into the right section of the patient’s chart without copy-pasting or switching screens. Whether you use Epic, Cerner or AthenaHealth, the integration keeps your documentation flow smooth and hassle-free.
7. Human Oversight for Review and Edits
Even with all that automation, the final say stays with the doctor. You can review the AI’s note, make changes if needed, and approve it before it’s filed. This keeps your documentation legally sound and clinically accurate while saving time. Most reviews take just a minute or two – far less than starting from scratch.
Benefits of Using an AI Medical Scribe
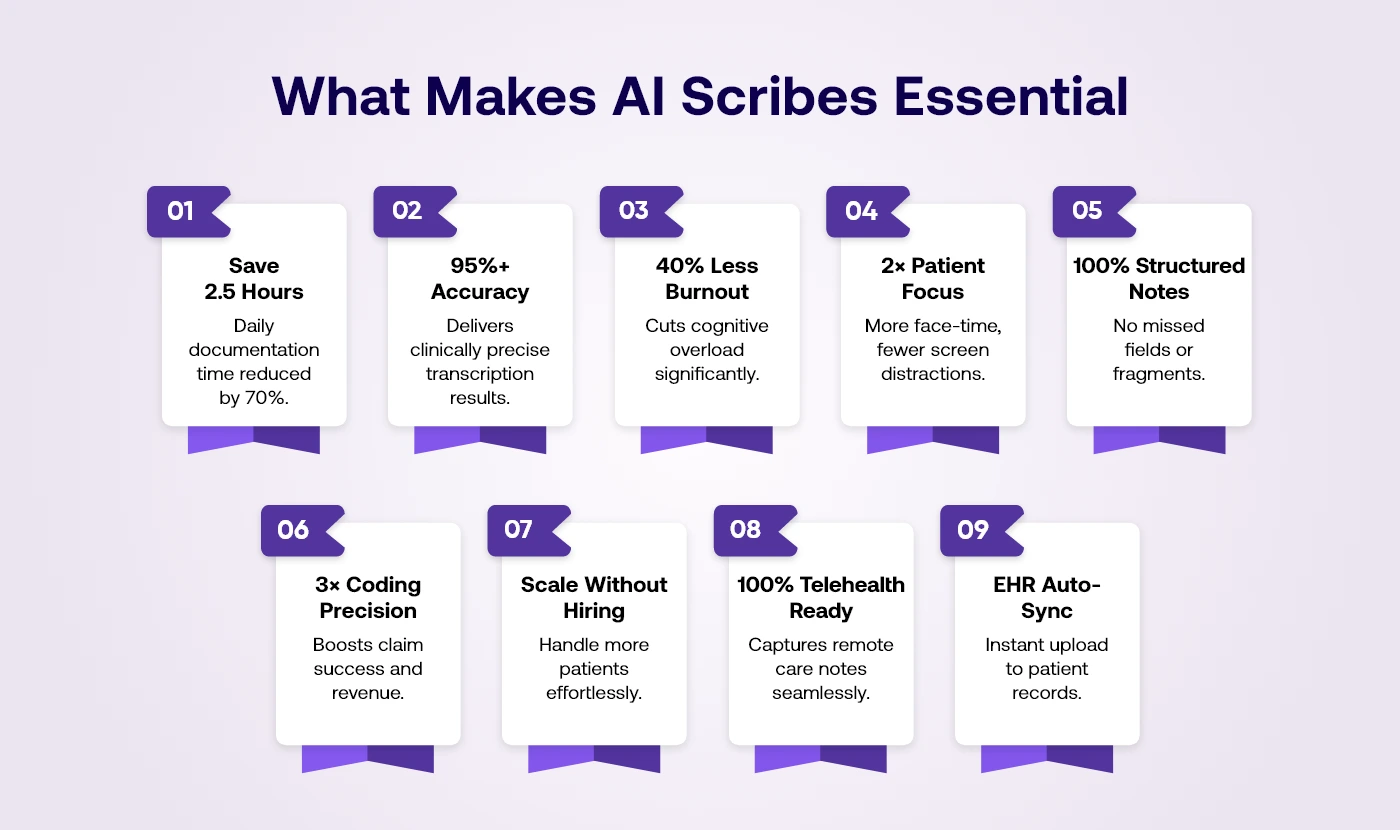
1. Saves Up to 2.5 Hours Daily
AI scribes significantly reduce documentation time, allowing physicians to focus more on care and productivity.
- Less after-hours documentation means faster shift wrap-up for doctors.
- Shorter gaps between appointments increases clinic throughput naturally.
- Enables physicians to end clinic days without staying late.
- More focus on patient care less on charting overhead.
- Reduces appointment delays caused by documentation overload.
2. Reduces Mental Load & Burnout
By handling repetitive tasks, AI scribes help reduce physician fatigue and emotional exhaustion long-term.
- Fewer late nights finishing charts from a packed clinic day.
- Offloads mental clutter from constantly toggling between EHR fields.
- Boosts focus and clarity during patient consultations.
- Helps prevent early burnout among newer healthcare providers.
- Aligns with wellness goals promoted in modern medical workplaces.
3. Coding Support & Revenue Optimization
AI scribes ensure accurate medical coding helping practices improve billing outcomes and reduce claim denials.
- Captures billable events doctors might forget to record manually.
- Flags missing codes or inconsistent documentation during the visit.
- Enhances documentation for audits, insurance reviews and compliance.
- Reduces claim denials from vague or incorrect chart entries.
- Turns documentation accuracy into real measurable revenue growth.
4. Improves Patient Engagement
With documentation automated, clinicians can fully focus on patients – leading to better trust and satisfaction.
- Sustained eye contact builds more trust during appointments.
- Fewer typing interruptions improves patient comfort and connection.
- More natural dialogue without structured dictation formats.
- Better memory recall from focused uninterrupted conversations.
- Improves long-term patient loyalty and clinical rapport.
5. Improves Documentation Quality
AI scribes structure every note clearly and completely ensuring no important detail gets left out.
- Reduces vague language and fragmented entries in EHR notes.
- Enforces structured note-taking across all provider types.
- Ensures clinical details aren’t missed or forgotten post-visit.
- Improves care handoff with clearer patient history and context.
- Supports long-term legal protection through consistent documentation practices.
6. Enables Scalable Practice Growth
Practices can grow without increasing admin burden thanks to automation that adapts to patient volume.
- Absorbs admin load without increasing headcount or overtime.
- Supports multi-specialty workflows without added onboarding effort.
- Ideal for scaling telehealth, urgent care or group practices.
- Reduces training time for new documentation support staff.
- Increases daily efficiency while protecting clinician bandwidth.
7. Enhanced Accuracy & Risk Reduction
AI scribes reduce documentation errors, ensuring accurate, compliant and audit-ready clinical notes every time.
- Ensures ICD and CPT codes align with spoken documentation.
- Reduces likelihood of malpractice due to missing documentation.
- Maintains accurate symptom-to-diagnosis mapping in every visit.
- Tracks timeline and details for legally compliant medical notes.
- Improves quality scores used for reimbursements and certifications.
8. Support for Telemedicine and Remote Care
AI scribes work seamlessly across virtual care settings, ensuring consistent documentation in every patient interaction.
- Transcribes virtual visits with the same accuracy as in-person.
- Works across mobile, desktop or browser-based telehealth tools.
- Helps remote care providers document thoroughly and in real time.
- Integrates telehealth notes directly into the central EHR system.
- Makes virtual care documentation fast, easy and fully compliant.
9. Seamless EHR Integration
AI scribes connect with EHR systems, streamlining data entry and reducing workflow interruptions for providers.
- Syncs final notes instantly to the patient’s health record.
- Reduces toggling between windows, platforms, or systems daily.
- Eliminates redundant data entry or manual documentation rework.
- Supports HL7/FHIR standards for smooth health system compatibility.
- Boosts charting speed without compromising on EHR data quality.
Challenges and How To Overcome Them
Let’s be honest: no technology—no matter how intelligent—is flawless. When it comes to using AI in healthcare, concerns naturally arise. From accuracy and data privacy to the fear of dehumanizing the care experience, clinicians want to know that the benefits outweigh the risks.
But here’s the good news: AI scribes are evolving fast, and when built with clinical precision, they can address most challenges head-on. That’s exactly where Scribeflo comes in.
Let’s explore the top concerns and how Scribeflo solves them.
Concern: Is AI Accurate Enough for Medical Documentation?
Accuracy is the foundation of clinical care. If AI scribes miss key symptoms, misinterpret a diagnosis, or document incomplete data it could have serious consequences. This is a valid concern for any healthcare provider.
How Scribeflo solves it:
Scribeflo, trained on 10M+ clinical conversations across 20+ specialties, goes beyond transcription by using medical NLP to understand context, diagnoses, and treatment logic. It delivers over 90% accuracy—even in fast-paced settings—adapts to accents and speech styles and always provides drafts for human review before EHR submission.
Concern: Is My Patient Data Truly Safe?
When AI systems process sensitive patient data, security and compliance become non-negotiable. Providers must ensure that Protected Health Information (PHI) is never exposed, misused, or stored without consent.
How Scribeflo solves it:
Scribeflo ensures data security with HIPAA-compliant architecture and AES-256 encryption. It follows a zero-retention policy by default—processing PHI in real time without storing it. With GDPR, SOC 2, and HL7 compliance and strict access controls, Scribeflo keeps your patients’ data fully protected and confidential at every step.
Concern: Will AI Replace Human Clinical Judgment?
Some clinicians worry that relying on an AI scribe might reduce their involvement in the documentation process or dilute the personal nature of their notes. After all medicine is both a science and an art.
How Scribeflo solves it:
Scribeflo supports – not replaces – human judgment. It automates tasks like transcription, structuring, and coding, while clinicians remain in full control. Doctors can review, edit, and finalize every note before submitting it to the EHR. Think of Scribeflo as your digital co-pilot – you focus on care, it handles the documentation workload.
How Scribeflo Helps?
Scribeflo is more than just an AI scribe – it’s a complete documentation automation platform designed around real clinical workflows. It transcribes live or recorded conversations into structured SOAP notes, adapts to each provider’s style, and syncs across devices – even offline.
With custom AI models for 20+ specialties, speaker differentiation, smart editing tools and HIPAA/SOC 2 compliance, Scribeflo eliminates the chaos of after-hours charting. Teams can collaborate securely, admins manage access and backups, and clinics maintain consistent, accurate, and audit-ready notes.
Clinicians now save up to 60% of documentation time, with 94% of users reporting higher accuracy and satisfaction.
Scribeflo doesn’t just save time – it elevates care.
Final Thoughts: Your Notes Shouldn’t Take More Time Than Your Patients
Let’s face it – no one became a doctor to spend hours typing notes after every shift.
Yet that’s the daily reality for thousands of clinicians. Manual documentation isn’t just a time suck – it’s one of the top causes of burnout, reduced patient engagement and missed billing opportunities.
AI medical scribes are changing that.
They work quietly in the background, listen with precision and turn every clinical conversation into ready-to-review notes – without the clicking, coding or context-switching. The result? Better documentation. Faster workflows. Happier doctors. Safer patients.
But not all AI scribes are built the same.
Scribeflo was built by clinicians, for clinicians – trained on 10M+ real conversations, tuned for accuracy and ready to integrate without disrupting your workflow.
If you’re ready to spend less time typing and more time practicing medicine…
👉 Try Scribeflo free and see the change in your very next shift.
Your EHR shouldn’t slow you down. Let AI catch up – so you can move forward.
Frequently Asked Questions
No, you can speak normally—just like you would during any patient visit. The AI is trained to understand natural speech, different accents, and medical terms without needing you to slow down or change how you talk.
No, the AI only starts listening when the patient encounter begins. It doesn’t eavesdrop on personal or background chatter, and everything is encrypted and secure. You stay in full control of when it records.
You always get the final say. The system creates a draft, and you can easily review and edit it before it’s saved. It’s quick—usually just takes a minute or two—and ensures everything looks exactly the way you want.
Featured Blogs
Read our thoughts and insights on the latest tech and business trends
Top iPhone App Development Companies in USA in 2026
- February 18, 2026
- Mobile App Development
In a Nutshell The USA remains one of the strongest hubs for premium iPhone app development in 2026, especially for fintech, healthcare, retail, and SaaS brands. Choosing the right iOS partner goes beyond portfolios; the... Read more
How to Choose the Right AI Development Partner in the USA (Enterprise Guide 2026)
- February 12, 2026
- Artificial Intelligence
In a Nutshell Enterprise AI success starts with clear business goals, not vague plans like “we need AI.” The best AI development partners deliver real production systems, not just impressive demos or prototypes. Industry alignment... Read more
How AI Is Transforming Transport & Logistics Operations in Real Time
- February 10, 2026
- Artificial Intelligence Logistics & Transportation
In a Nutshell: AI in transport & logistics is enabling faster, smarter decision-making across fleets, warehouses, and supply chains. Real-time logistics optimization improves route planning, dispatching, and delivery efficiency as conditions change. AI-driven forecasting and... Read more